- Created by Amir Shehata, last modified on Feb 06, 2022
You are viewing an old version of this page. View the current version.
Compare with Current View Page History
« Previous Version 5 Next »
A year after the country’s first Covid-19 cluster, with 5 cases, was reported in Agra district, the Uttar Pradesh government has claimed that it was the first state to have introduced a large-scale “prophylactic and therapeutic” use of Ivermectin and added that the drug helped the state to maintain a lower fatality and positivity rate as compared to other states.
Citing the results from Agra in the month of May and June last year, following which the use of Ivermectin, a medicine to treat parasitic ailments, along with Doxycycline was introduced as a protocol across the state for both prophylactic as well as treatment purposes, the state Health Department said it would conduct a controlled study once the second wave of the pandemic subsides.
The state Health Department introduced Ivermectin as prophylaxis for close contacts of Covid patients, health workers as well as for the treatment of the patients themselves through a government order on August 6, 2020, after a committee headed by the Director General, Medical and Health Services, gave it the go ahead.
“Uttar Pradesh was the first state in the country to introduce large-scale prophylactic and therapeutic use of Ivermectin. In May-June 2020, a team at Agra, led by Dr Anshul Pareek, administered Ivermectin to all RRT team members in the district on an experimental basis. It was observed that none of them developed Covid-19 despite being in daily contact with patients who had tested positive for the virus,” Uttar Pradesh State Surveillance Officer Vikssendu Agrawal said.
He added that based on the findings from Agra, the state government sanctioned the use of Ivermectin as a prophylactic for all the contacts of Covid patients and later cleared the administration of therapeutic doses for the treatment of such patients.
Claiming that timely introduction of Ivermectin since the first wave has helped the state maintain a relatively low positivity rate despite its high population density, he said, “Despite being the state with the largest population base and a high population density, we have maintained a relatively low positivity rate and cases per million of population”.
He said that apart from aggressive contact tracing and surveillance, the lower positivity and fatality rates may be attributed to the large-scale use of Ivermectin use in the state, adding that the drug has recently been introduced in the National Protocol for Covid treatment and management. “Once the second wave subsides, we would conduct our own study as there has been an emerging body of evidence to substantiate our timely use of Ivermectin from the first wave itself,” Vikasendu told The Indian Express.
Agra District Magistrate Prabhu N Singh also attributed the state’s relative success in keeping the Covid numbers down to the timely nod to the use of Ivermectin as a prophylactic. He added that government doctor Anshul Pareek had approached him last year citing use of the medicine abroad.
“We reported the first Covid-19 cluster in the country after five members of a family, who had returned from Italy, tested positive. Soon, the virus spread, with a large number of police personnel getting affected. Doctor Pareek approached me with a request to introduce Ivermectin on an experimental basis. I was told there are no risks involved with the use of the drug,” Singh told The Indian Express.
He said the district administration had formed small groups of personnel from the same police station as well staffers at his office. “We introduced it (Ivermectin) for three days, 12 mg as advised in the national guidelines at the time, followed by tests on the fourth or fifth day. We introduced it in the jail as well and the results helped us reduce positivity to a great extent, following which Additional Chief Secretary Health Amit Mohan formed a committee to access its usage and it was finally introduced in the state’s Covid management protocol in 2020 itself,” Singh said.
Ivermectin Prophylaxis Used for COVID-19: A Citywide, Prospective, Observational Study of 223,128 Subjects Using Propensity Score Matching
Lucy Kerr, Flavio A. Cadegiani, Fernando Baldi, Raysildo B. Lobo, Washington Luiz O. Assagra, Fernando Carlos Proença, Pierre Kory, Jennifer A. Hibberd, Juan J. Chamie-Quintero
Published: January 15, 2022 (see history)
DOI: 10.7759/cureus.21272
Cite this article as: Kerr L, Cadegiani F A, Baldi F, et al. (January 15, 2022) Ivermectin Prophylaxis Used for COVID-19: A Citywide, Prospective, Observational Study of 223,128 Subjects Using Propensity Score Matching. Cureus 14(1): e21272. doi:10.7759/cureus.21272
Abstract
Background: Ivermectin has demonstrated different mechanisms of action that potentially protect from both coronavirus disease 2019 (COVID-19) infection and COVID-19-related comorbidities. Based on the studies suggesting efficacy in prophylaxis combined with the known safety profile of ivermectin, a citywide prevention program using ivermectin for COVID-19 was implemented in Itajaí, a southern city in Brazil in the state of Santa Catarina. The objective of this study was to evaluate the impact of regular ivermectin use on subsequent COVID-19 infection and mortality rates.
Materials and methods: We analyzed data from a prospective, observational study of the citywide COVID-19 prevention with ivermectin program, which was conducted between July 2020 and December 2020 in Itajaí, Brazil. Study design, institutional review board approval, and analysis of registry data occurred after completion of the program. The program consisted of inviting the entire population of Itajaí to a medical visit to enroll in the program and to compile baseline, personal, demographic, and medical information. In the absence of contraindications, ivermectin was offered as an optional treatment to be taken for two consecutive days every 15 days at a dose of 0.2 mg/kg/day. In cases where a participating citizen of Itajaí became ill with COVID-19, they were recommended not to use ivermectin or any other medication in early outpatient treatment. Clinical outcomes of infection, hospitalization, and death were automatically reported and entered into the registry in real time. Study analysis consisted of comparing ivermectin users with non-users using cohorts of infected patients propensity score-matched by age, sex, and comorbidities. COVID-19 infection and mortality rates were analyzed with and without the use of propensity score matching (PSM).
Results: Of the 223,128 citizens of Itajaí considered for the study, a total of 159,561 subjects were included in the analysis: 113,845 (71.3%) regular ivermectin users and 45,716 (23.3%) non-users. Of these, 4,311 ivermectin users were infected, among which 4,197 were from the city of Itajaí (3.7% infection rate), and 3,034 non-users (from Itajaí) were infected (6.6% infection rate), with a 44% reduction in COVID-19 infection rate (risk ratio [RR], 0.56; 95% confidence interval (95% CI), 0.53-0.58; p < 0.0001). Using PSM, two cohorts of 3,034 subjects suffering from COVID-19 infection were compared. The regular use of ivermectin led to a 68% reduction in COVID-19 mortality (25 [0.8%] versus 79 [2.6%] among ivermectin non-users; RR, 0.32; 95% CI, 0.20-0.49; p < 0.0001). When adjusted for residual variables, reduction in mortality rate was 70% (RR, 0.30; 95% CI, 0.19-0.46; p < 0.0001). There was a 56% reduction in hospitalization rate (44 versus 99 hospitalizations among ivermectin users and non-users, respectively; RR, 0.44; 95% CI, 0.31-0.63; p < 0.0001). After adjustment for residual variables, reduction in hospitalization rate was 67% (RR, 0.33; 95% CI, 023-0.66; p < 0.0001).
Conclusion: In this large PSM study, regular use of ivermectin as a prophylactic agent was associated with significantly reduced COVID-19 infection, hospitalization, and mortality rates.
Introduction
Ivermectin has been demonstrated to have not only extensive anti-parasitic actions [1,2], but also anti-viral, anti-bacterial, and anti-protozoan properties. Ivermectin has been long proposed for use as a repurposed antiviral agent [3-6]. Indeed, antiviral effects of ivermectin have been reported against both RNA and DNA types of viruses, including HIV-1, yellow fever, Japanese encephalitis, tick-borne encephalitis, West Nile, Zika, dengue fever, chikungunya, Venezuelan equine encephalitis, and the pseudorabies virus [3,5,7,8], as well as functioning in regulation of proteins involved in antiviral responses [8].
Additional actions of ivermectin described include agonism activity to the liver X receptor (LXR) and farnesoid X receptor (FXR), with multiple potential metabolic benefits [9,10]; neuronal regeneration [11,12], prevention of muscle hypoxia [13], and actions on specific sites, including interferon (INF) [14], nuclear factor-κB (NF-κB), lipopolysaccharide (LPS) [15], and Janus kinase/signal transducer and activator of transcription (JAK-STAT) and PAI-1 pathway [16,17]; generation of P21 activated kinase 1 (PAK-1) [18,19]; reduction of interleukin-6 (IL-6) levels [15]; allosteric modulation of P2X4 receptor [20]; inhibition of high mobility group box 1 (HMGB1) [21,22]; and suppression of mucus hypersecretion, diminished recruitment of immune cells, and production of cytokines in the lung [23]. Ivermectin is also described to induce T helper 1 cell (Th1)-type immune response against protozoan infections [24], and anti-coagulant action through binding to the S protein of some viruses [25].
The hypothesis that ivermectin could be protective against coronavirus disease 2019 (COVID-19) is substantiated by its multi-pathway, anti-inflammatory effects [15,26], and multi-antiviral mechanisms. COVID-19 pathogenesis is largely understood as an inflammation-mediated hemagglutinating infection disrupting pulmonary, vascular, and endothelial systems, leading to a multi-systemic disease. In vitro and in silico, ivermectin has demonstrated anti-severe acute respiratory syndrome coronavirus 2 activity through more than 20 direct and indirect mechanisms [2,27,28].
Ivermectin has demonstrated preliminary protective effects against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in terms of reducing times to clinical recovery and rates of disease progression and mortality [2,29,30]. However, more robust studies with larger sample sizes are still recommended to confirm the possible beneficial effects of ivermectin in COVID-19.
Since the onset of the COVID-19 pandemic, the use of inexpensive options based on a consistently beneficial signal of efficacy, a well-established safety profile, and favorable cost-effectiveness, ivermectin is a highly attractive intervention for the patient-centered medicine practiced by frontline clinicians, with use aligning strongly with the bioethical principles for medical practice outlined in Article 36 of the Declaration of Helsinki [31].
However, despite this favorable risk/benefit profile and absence of therapeutic alternatives, ivermectin is yet to be approved for prophylaxis and treatment of COVID-19 by agencies throughout the world, including FDA (USA), European Medicines Agency (EMA; Europe), and ANVISA (Agência Nacional de Vigilância Sanitária - Brazilian Health Regulatory Agency; Brazil).
The ability to prescribe ivermectin or any other off-label drug for COVID-19 has long been at the discretion of frontline physicians once all risks, uncertainties, potential benefits, and patients’ rights are exposed, and informed consent has been obtained. Of particular note, in Brazil, this follows the medical autonomy to determine the best therapeutic strategies for individuals, as per the Medical Code of Ethics of the Brazilian Board of Medical Doctors, the Federal Council of Medicine - Conselho Federal de Medicina (CFM), that determines the obligations and rights of medical doctors in Brazil [32].
Since vaccines for COVID-19 were not available in Brazil until 2021, and because of the lack of prophylactic alternatives in the absence of vaccines, Itajaí, a city in the southern Brazilian state of Santa Catarina, initiated a population-wide government program for COVID-19 prophylaxis. The medical-focused decision parameters established are based on the distribution of ivermectin to whole populations in different countries. To ensure the safety of the population, a well-controlled computer program was developed to compile and maintain all relevant demographic and clinical data (detailed in the Materials & Methods section). The use of ivermectin was optional and based on patients’ preferences, given its benefits as a preventative agent was unproven.
This study’s objective is to assess the impact on important clinical outcomes when ivermectin is used as prophylaxis for COVID-19. The prophylaxis program occurred in addition to the standard non-pharmacological strategies of masking and social distancing, as part of a citywide program conducted in outpatient settings.
Materials & Methods
Study population
This was a prospective, observational study. Although study design, institutional review board (IRB) approval, and data analysis occurred after completion of the voluntary prophylaxis program, all data were collected prospectively in real time with mandated reporting to the registry of all events as they occurred during the citywide governmental COVID-19 prevention with ivermectin program, from July 2020 to December 2020, developed in the city of Itajaí, in the state of Santa Catarina, Brazil. Demographic and clinical data were reported from medical records of patients followed in a large outpatient setting (a provisional outpatient clinic set in the Convention Center of Itajaí) and several secondary outpatient settings, as part of the universal health system (Sistema Único de Saúde [SUS]).
The objective was to determine the number of patients affected by COVID-19 (positivity rate of reverse transcription-polymerase chain reaction [RT-PCR] for SARS-CoV-2), risk of death due to COVID-19 (whether infected or not), and COVID-19 mortality rate (risk of death from COVID-19) of those who used and did not use ivermectin prophylactically for COVID-19. These data were stratified by age, sex, presence of comorbidities, and correlated demographic characteristics.
The present retrospective analysis of the prospectively collected data was approved by the National Research Ethics Council (CONEP) under the number 4.821.082 with the project number CAAE: 47124221.2.0000.5485. Although study design, IRB approval, and data analysis occurred after completion of the voluntary prophylaxis program, all data were collected prospectively in real-time with mandated reporting to the registry of all events as they occurred during the citywide governmental COVID-19 prevention with ivermectin program, from July 7, 2020, to December 2, 2020, developed in the city of Itajaí, in the state of Santa Catarina, Brazil.
Study procedures and data collection
Optional, voluntary prophylactic use of ivermectin was offered to patients during regular medical visits between July 7, 2020, and December 2, 2020, in 35 different sites, including 34 local SUS health centers and a large temporary patient setting 24/7. Doctors working in these sites were free to prescribe ivermectin prophylactically. Subjects that did not use ivermectin either refused or their primary care physicians opted not to offer ivermectin.
To avoid underreported data, strict procedure sequencing was followed: (1) registration and recording of patient data, documented by assistants; (2) weighing subjects (subject's weight was essential to calculate the appropriate dose of ivermectin); (3) brief medical evaluation of past medical history, comorbidities, use of medications, and contraindications to drugs; and (4) medical prescription with prophylactic doses of ivermectin (within recommended usual, safe doses of ivermectin), according to medical judgment and following a subject’s informed consent related to potential benefits, risks, and side effects. All details of this citywide program and campaign had been previously agreed upon between the city local department of the National Healthcare System (SUS), city mayor, and local public prosecutors.
Regarding drug interactions with ivermectin, the use of warfarin was a contraindication for prophylaxis with ivermectin due to drug interactions. Subjects under chronic use of glucocorticoids, protease inhibitors, and anti-epileptics were recommended to schedule regular medical visits every six to eight weeks. Subjects were recommended to inform medical doctors about the use of ivermectin, in case one or more of the following medications were prescribed: warfarin, azithromycin, dexamethasone, prednisone, or prednisolone (hydrocortisone or cortisone are not commercially available in regular pharmacies in Brazil).
The following variables were analyzed: (1) age, (2) sex, (3) previous diseases (myocardial infarction [MI] and stroke), (4) pre-existing comorbidities (type 2 diabetes [T2D], asthma, chronic obstructive pulmonary disease [COPD], hypertension, dyslipidemia, cardiovascular diseases [CVD], cancer [any type], and other pulmonary diseases), and (5) smoking. Variables were adjusted as confounding factors and used as variables for balancing and matching groups for propensity score matching (PSM).
Patients who presented signs or the diagnosis of COVID-19 before July 7, 2020, were excluded from the sample. Other exclusion criteria were contraindications to ivermectin and subjects below 18 years of age. The dose and frequency of ivermectin treatment was 0.2 mg/kg/day; i.e., giving one 6 mg tablet for every 30 kg for two consecutive days every 15 days.
During the study, subjects who were diagnosed with COVID-19 underwent a specific medical visit to assess COVID-19 clinical manifestations and severity. All subjects were recommended not to use ivermectin, nitazoxanide, hydroxychloroquine, spironolactone, or any other drug claimed to be effective against COVID-19. The city did not provide or support any specific pharmacological outpatient treatment for subjects infected with COVID-19.
They were questioned for the presence of common COVID-19 symptoms. These included chills, high-grade fever, cough, myalgia, fatigue, anosmia, ageusia, sore throat, headache, nasal congestion, sneeze, runny nose, hemoptysis, nausea, vomiting, abdominal pain, diarrhea, cutaneous rash, arthralgia, chest pain, eye pain and pinkeye, and presence of alert signs, including shortness of breath, signs of hypoxia, signs of coagulation abnormalities, and an altered level of consciousness. Systolic and diastolic blood pressure, heart rate, respiratory rate, oxygen saturation, and axillary temperature were measured. The same signs and symptoms and vital signs were collected at each following medical visit during COVID-19. Individual data were compiled and reviewed by the researchers.
Registry data of all patient records from the city of Itajaí between July 7, 2020, and December 2, 2020, including those who used ivermectin and did not use ivermectin were reviewed. All subjects who tested positive for COVID-19 in the city of Itajaí during the study were considered for this analysis. Of the infected subjects, two groups were considered: subjects who used ivermectin prophylactically (treated group) and subjects who did not use ivermectin prophylactically (untreated group). Missing data from patients were clarified with patients or relatives directly, via phone or in person, by the investigators. Since this is a citywide program, all recorded data must have matched the exact number of COVID-19 cases and deaths of the city. This strict interval avoids differences in terms of periods of exposure.
Due to the uncertainty of reinfection with COVID-19, subjects with a history of previous COVID-19 did not participate in the program although they were still permitted to use ivermectin prophylactically. Limiting parameters of the government system allowed the recording of a first episode of COVID-19 infection only. Subjects below 18 years old and subjects with a diagnosis of COVID-19 before July 7, 2020, were excluded from all datasets and analyses.
From the registry of the city population (223,128 inhabitants), subjects below 18 years old (61,583 subjects) were removed. Of the 161,545 subjects above 18 years old from the city of Itajaí, we removed the 1,984 COVID-19 cases that occurred before July 7, 2020, and 159,561 subjects remained. Subjects above 18 years old were considered those who were born before June 30, 2002.
A total of 147,223 subjects participated in the program of ivermectin prophylaxis used for COVID-19. Of these, 24,304 subjects were below 18 years old. Of the 122,919 ivermectin users above 18 years old, 8,346 were from other cities, and 728 had COVID-19 before July 7, 2020, although they used ivermectin afterward. In total, 113,845 subjects that participated in the program remained in the dataset. The 45,716 non-participants, remaining subjects among the 159,561 subjects, were considered as the ivermectin non-users.
Finally, citywide COVID-19 hospitalization and mortality rates of Itajaí were compared between the period before the program (before July 7, 2020) and during the program (between July 7, 2020, and December 2, 2020) aiming to evaluate whether a program of prophylaxis with ivermectin for COVID-19 would cause a positive impact in the overall numbers of the city, despite only partial adoption. Chances of dying of COVID-19 in the overall population, according to use or non-use of ivermectin (irrespective of COVID-19 infection) were only calculated prior to matching. Conversely, the mortality rate among those who were infected by the SARS-CoV-2 was calculated for both pre and post-matched cohorts.
Hospitalization and mortality rates before matching groups, the mortality rate in subpopulations before and after PSM, and the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist are presented in the Appendix.
Statistical analysis
The full underlying data for the present analysis were analyzed by two independent statisticians, and discrepancies were evaluated by a third statistics expert. In this outpatient study of those who tested positive for SARS-CoV-2, the mortality rate was evaluated according to each parameter that was adjusted against other variables (for multivariate regression analysis) and used for balancing and matching groups, including age intervals, sex, history of smoking, prophylactic ivermectin use, T2D, asthma, COPD, cardiovascular diseases and other pulmonary diseases, hypertension, current cancer (any type), and history of stroke and/or MI.
Before matching, a generalized linear mixed model was employed, assuming the binomial distribution for the residues and including the fixed classificatory effects of each of these parameters. Age intervals were adjusted for the evaluation of ivermectin prophylactic use as an independent predictor of death from COVID-19. Unadjusted and multivariate Poisson-adjusted probabilities to survive from COVID-19 (p-value), according to each parameter, were provided.
PSM was performed for mortality risk between ivermectin and non-ivermectin users. COVID-19 infection rate and risk of dying were also calculated for variables. After PSM, a second adjustment ("double adjustment") with multivariate linear regression was performed for residual variables [33,34].
There were no missing data since the registry system design mandated that all data variables be filled to be formally included in the registry. Only erroneously entered (illogical) data were found. In such instances, a medical record review was performed to obtain accurate data. The program used for the analysis was the Statistical Analysis Software (SAS/STAT) (SAS Institute Inc., Cary, NC). For transparency reasons, two datasets of the 7,345 COVID-19 cases and the 113,845 participating subjects considered for the present analysis will be made public upon peer-reviewed publication.
Results
A detailed description of the data considered for the present analysis is illustrated in Figure 1. Of the 220,517 citizens of Itajaí without COVID-19 until July 7, 2020, 159,561 were above 18 years old. Of the 159,561 citizens above 18 years old without COVID-19 until July 7, 2020, 113,845 (71.3% of the population above 18 years old) received ivermectin before being infected by COVID-19. A total of 45,716 citizens (28.7%) did not receive or did not want to receive ivermectin during the program, including as a prophylactic or as a treatment after having COVID-19.
Figure 1: Underlying data for the study on ivermectin prophylaxis used for COVID-19.
Of the 113,845 prophylaxed subjects from the city of Itajaí, 4,197 had a positive RT-PCR SARS-CoV-2 (3.7% infection rate), while 3,034 of the 37,027 untreated subjects had positive RT-PCR SARS-CoV-2 (6.6% infection rate), a 44% reduction in COVID-19 infection rate (risk ratio [RR], 0.56; 95% confidence interval (95% CI), 0.53-0.58; p < 0.0001). An addition of 114 subjects who used ivermectin and were infected were originally from other cities but were registered as part of the program, in a total of 4,311 positive cases among ivermectin users. For the present analysis, the 4,311 positive cases among subjects that used ivermectin and 3,034 cases among subjects that did not use ivermectin were considered. After PSM, two cohorts of 3,034 subjects were created.
Baseline characteristics of the 7,345 subjects included prior to PSM and the baseline characteristics of the 6,068 subjects in the matched groups are shown in Table 1. Prior to PSM, ivermectin users had a higher percentage of subjects over 50 years old (p < 0.0001), higher prevalence of T2D (p = 0.0004), hypertension (p < 0.0001), and CVD (p = 0.03), and a higher percentage of Caucasians (p = 0.004), than non-users. After PSM, all baseline parameters were similar between groups. Figure 2 summarizes the main findings of this study.
| Pre-matching | Propensity score-matched | ||||||
| Overall (n = 7,345) | Ivermectin users (n = 4,311) | Non-ivermectin users (n = 3,034) | p-value | Overall (n = 6,068) | Ivermectin users (n = 3,034) | Non-ivermectin users (n = 3,034) | |
| Age | |||||||
| Mean ± SD | 42.0 ± 14.7 | 43.5 ± 14.9 | 39.8 ± 14.2 | <0.0001 | 39.7 ± 14.0 | 3967 ± 13.8 | 39.8 ± 14.2 |
| <30 years old | 1,730 (23.6%) | 886 (20.5%) | 844 (27.8%) | 1,691 (27.9%) | 844 (27.9%) | 847 (27.8%) | |
| 30-50 years old | 3,703 (50.4%) | 2,121 (49.2%) | 1,582 (52.2%) | 3,155 (52.0%) | 1,573 (51.9%) | 1,582 (52.1%) | |
| >50 years old | 1,912 (26.0%) | 1,304 (30.3%) | 608 (20.0%) | 1,222 (20,1%) | 614 (20.2%) | 608 (20.1%) | |
| Sex | 0.31 | ||||||
| Female | 3,983 (54.2%) | 2,359 (54.7%) | 1,624 (53.5%) | 3,231 (53.2%) | 1,607 (53.0%) | 1,624 (53.5%) | |
| Male | 3,362 (45.8%) | 1,952 (45.3%) | 1,410 (46.5%) | 2,837 (46.8%) | 1,427 (47.0%) | 1,410 (46.5%) | |
| Race | |||||||
| Caucasians | 5,437 (74.0%) | 3,245 (75.3%) | 2,192 (72.2%) | 0.004 | 4,398 (72.5%) | 2,206 (72.7%) | 2,192 (72.3%) |
| Afro-Brazilians | 209 (2.8%) | 109 (2.5%) | 100 (3.3%) | 0.052 | 193 (3.2%) | 93 (3.1%) | 100 (3.3%) |
| Mixed | 1,583 (22.6%) | 901 (20.9%) | 682 (22.5%) | 0.10 | 1,364 (22.5%) | 93 (3.1%) | 100 (3.3%) |
| Asian-Brazilians | 116 (1.6%) | 56 (1.3%) | 60 (2.0%) | 0.023 | 113 (1.9%) | 53 (1.8%) | 60 (2.0%) |
| Type 2 diabetes | 0.0004 | ||||||
| Yes | 214 (2.9%) | 151 (3.5%) | 63 (2.1%) | 141 (2.3%) | 78 (2.6%) | 63 (2.1%) | |
| No | 7,131 (97.1%) | 4,160 (96.5%) | 2,971 (97.9%) | 5,927 (97.7%) | 2,956 (97.4%) | 2,971 (97.9%) | |
| Asthma | 0.067 | ||||||
| Yes | 26 (0.3%) | 20 (0.5%) | 6 (0.2%) | 21 (0.3%) | 15 (0.5%) | 6 (0.2%) | |
| No | 7,319 (99.7%) | 4,291 (99.5%) | 3,028 (99.8%) | 6,047 (99.7%) | 3,019 (99.5%) | 3,028 (99.8%) | |
| COPD | 0.72 | ||||||
| Yes | 13 (0.2%) | 7 (0.2%) | 6 (0.2%) | 12 (0.2%) | 6 (0.2%) | 6 (0.2%) | |
| No | 7,332 (99.8%) | 4,304 (99.8%) | 3,028 (99.8%) | 6,056 (99.8%) | 3,028 (99.8%) | 3,028 (99.8%) | |
| Hypertension | <0.0001 | ||||||
| Yes | 528 (7.2%) | 362 (8.4%) | 166 (5.5%) | 343 (5.6%) | 177 (5.8%) | 166 (5.5%) | |
| No | 6,817 (92.8%) | 3,949 (91.6%) | 2,868 (94.5%) | 5,725 (94.4%) | 2,857 (94.2%) | 2,868 (94.5%) | |
| CVD | 0.03 | ||||||
| Yes | 56 (0.8%) | 41 (1.0%) | 15 (0.5%) | 32 (0.5%) | 17 (0.6%) | 15 (0.5%) | |
| No | 7,289 (99.2%) | 4,270 (99.0%) | 3,019 (99.5%) | 6,036 (99.5%) | 3,017 (99.4%) | 3,019 (99.5%) | |
| Other pulmonary diseases | 0.53 | ||||||
| Yes | 15 (0.2%) | 10 (0.2%) | 5 (0.2%) | 9 (0.1%) | 4 (0.1%) | 5 (0.1%) | |
| No | 7,330 (99.8%) | 4,301 (99.8%) | 3,029 (99.8%) | 6,059 (99.9%) | 3,030 (99.9%) | 3,029 (99.9%) | |
| Cancer (any type) | 0.66 | ||||||
| Yes | 32 (0.4%) | 20 (0.5%) | 12 (0.4%) | 22 (0.4%) | 10 (0.3%) | 12 (0.4%) | |
| No | 7,313 (99.6%) | 4,291 (99.5%) | 3,023 (99.6%) | 6,046 (99.6%) | 3,024 (99.7%) | 3,022 (99.6%) | |
| Current smoking | 0.76 | ||||||
| Yes | 110 (1.5%) | 63 (1.5%) | 47 (1.5%) | 95 (1.6%) | 48 (1.6%) | 47 (1.6%) | |
| No | 7,235 (98.5%) | 4,248 (98.5%) | 2,987 (98.5%) | 5,973 (98.4%) | 2,986 (98.4%) | 2,987 (98.4%) | |
| History of MI | 0.26 | ||||||
| Yes | 15 (0.2%) | 11 (0.3%) | 4 (0.1%) | 8 (0.1%) | 4 (0.1%) | 4 (0.1%) | |
| No | 7,330 (99.8%) | 4,300 (99.7%) | 3,030 (99.9%) | 6,060 (99.9%) | 3,030 (99.9%) | 3,030 (99.9%) | |
| History of stroke | 0.56 | ||||||
| Yes | 21 (0.3%) | 11 (0.3%) | 10 (0.3%) | 21 (0.4%) | 11 (0.4%) | 10 (0.3%) | |
| No | 7,324 (99.7%) | 4,300 (99.7%) | 3,024 (99.7%) | 6,047 (99.6%) | 3,023 (99.6%) | 3,024 (99.7%) | |
Table 1: Baseline characteristics of subjects enrolled in the study before matching and after propensity score matching.
COPD = chronic obstructive pulmonary disease; CVD = cardiovascular disease; MI = myocardial infarction; SD = standard deviation.
Figure 2: Summary of the findings.
Hospitalization and mortality rates in ivermectin users and non-users in propensity score-matched analysis
As described in Table 2, after employing PSM, of the 6,068 subjects (3,034 in each group), there were 44 hospitalizations among ivermectin users (1.6% hospitalization rate) and 99 hospitalizations (3.3% hospitalization rate) among ivermectin non-users, a 56% reduction in hospitalization rate (RR, 0.44; 95% CI, 0.31-0.63). When adjustment for variables was employed, the reduction in hospitalization rate was 67% (RR, 0.33; 95% CI, 023-0.66; p < 0.0001).
| Overall | IVM users | Non-IVM users | PSM mortality risk ratio (95% CI) and p-value [p] | Adjusted PSM mortality risk ratio (95% CI) and p-value [p] | ||
| COVID-19 infection | Infected population (n) | 6,068 | 3,034 | 3,034 | - | - |
| COVID-19 hospitalization | Hospitalization due to COVID-19 | 143 | 44 | 99 | - | - |
| Hospitalization rate* (in case of COVID-19) (%) | 2.3% | 1.6% | 3.3% | 0.44 (0.31-0.63) [<0.0001] | 0.33 (0.23-0.46) [<0.0001] | |
| COVID-19 death | COVID-19 deaths (n)** | 104 | 25 | 79 | - | - |
| Mortality rate (among infected subjects) (%) | 1.7% | 0.8% | 2.6% | 0.32 (0.20-0.49) [<0.0001] | 0.30 (0.19-0.46) [<0.0001] |
Table 2: Propensity score-matched hospitalization and mortality rate among ivermectin users and non-users.
IVM = ivermectin; PSM = propensity score matching. * Only subjects hospitalized in public hospitals. ** All deaths, including from public and private hospitals, and in-home.
There were 25 deaths among ivermectin users (0.8% mortality rate) and 79 deaths among non-ivermectin users (2.6% mortality rate), a 68% reduction in mortality rate (RR, 0.32; 95% CI, 0.20-0.49). When PSM was adjusted, reduction in mortality rate was 70% (RR, 0.30; 95% CI, 0.19-0.46; p < 0.0001).
Determinants of COVID-19 mortality through propensity score-matched analysis
Table 3 describes the resulting risk factors for COVID-19 death amongst the overall population through PSM analysis. Risk factors for mortality in COVID-19 included aging (p < 0.0001), male sex (p = 0.015), T2D (p < 0.0001), hypertension (p < 0.0001), asthma (p = 0.011), COPD (p < 0.0001), other pulmonary diseases (p = 0.048), history of MI (p = 0.034), and history of stroke (p < 0.0001). To detect independent risk factors, post-PSM adjustment for variables showed that ivermectin (p < 0.0001; 70% reduction in mortality risk) and female sex (p = 0.022; 38% reduction in mortality risk) were protectors, whereas T2D (p = 0.041; 79% increase in mortality risk), hypertension (p = 0.008; 98% increase in mortality risk), and, marginally, other pulmonary diseases (p = 0.061; 468% increase in mortality risk) and history of stroke (p = 0.054; 97% increase in mortality risk) were identified as independent risk factors.
| Propensity score-matched groups | ||||
| Variable | Overall (n = 6,068) | Death (%) | Unadjusted COVID-19 mortality risk ratio and p-value [p] | Multivariate adjusted COVID-19 mortality risk ratio and p-value [p] |
| Ivermectin use - n (%) | 0.32 (0.20-0.49) [<0.0001] | 0.30 (0.19-0.46) [<0.0001] | ||
| Yes | 3,034 | 25 (0.8%) | ||
| No | 3,034 | 79 (2.6%) | ||
| Age - n (%) | [<0.0001] | [<0.0001] | ||
| <30 years old | 1,691 | 1 (0.1%) | ||
| 30-50 years old | 3,155 | 12 (0.4%) | ||
| >50 years old | 1,222 | 91 (7.4%) | ||
| Sex - n (%) | 0.62 (0.42-0.91) [0.015] | 0.64 (0.44-0.93) [0.022] | ||
| Female | 3,231 | 43 (1.3%) | ||
| Male | 2,837 | 61 (2.2%) | ||
| Race - n (%) | [0.24] | [0.44] | ||
| Caucasians | 4,398 | 79 (1.8%) | ||
| Afro-Brazilians | 193 | 6 (3.1%) | ||
| Mixed | 1.364 | 17 (1.3%) | ||
| Asian-Brazilians | 113 | 2 (1.9%) | ||
| Type 2 diabetes - n (%) | 10.0 (6.32-15.8) [<0.0001] | 1.79 (1.03-3.12) [0.041] | ||
| Yes | 141 | 20 (14.2%) | ||
| No | 5,927 | 84 (1.4%) | ||
| Hypertension - n (%) | 8.83 (5.99-13.0) [< 0.0001] | 1.98 (1.19-3.30) [0.008] | ||
| Yes | 343 | 36 (10.5%) | ||
| No | 5,725 | 68 (1.2%) | ||
| Asthma - n (%) | 5.64 (1.49-21.4) [0.011] | 1.74 (0.52-5.81) [0.36] | ||
| Yes | 21 | 2 (9.5%) | ||
| No | 6,047 | 102 (1.7%) | ||
| COPD - n (%) | 15.0 (5.52-40.7) [<0.0001] | 1.71 (0.68-4.31) [0.25] | ||
| Yes | 12 | 3 (25.0%) | ||
| No | 6,056 | 101 (1.7%) | ||
| Cardiovascular diseases - n (%) | 7.54 (2.96-19.3) [<0.0001] | 1.22 (0.44-3.37) [0.70] | ||
| Yes | 32 | 4 (12.5%) | ||
| No | 6,036 | 100 (1.7%) | ||
| Other pulmonary diseases - n (%) | 6.54 (1.02-41.9) [0.048] | 5.68 (0.92-35.0) [0.061] | ||
| Yes | 9 | 1 (11.1%) | ||
| No | 6,059 | 103 (1.7%) | ||
| Cancer (any type) - n (%) | 2.67 (0.39-18.3) [0.32] | 1.97 (0.30-12.9) [0.48] | ||
| Yes | 22 | 1 (4.6%) | ||
| No | 6,046 | 103 (1.7%) | ||
| Current smoking - n (%) | 1.23 (0.31-4.92) [0.77] | 0.36 (0.08-1.70) [0.20] | ||
| Yes | 95 | 2 (2.1%) | ||
| No | 5,973 | 102 (1.7%) | ||
| History of MI - n (%) | 7.35 (1.16-46.5) [0.034] | 1.91 (0.17-21.6) [0.60] | ||
| Yes | 8 | 1 (12.5%) | ||
| No | 6,060 | 103 (1.7%) | ||
| History of stroke - n (%) | 17.6 (8.72-35.7) [< 0.0001] | 1.97 (0.99-3.92) [0.054] | ||
| Yes | 21 | 6 (28.6%) | ||
| No | 6,047 | 98 (1.6%) | ||
Table 3: Propensity score-matched COVID-19 mortality rate according to each characteristic in the overall population, ivermectin users, and non-users.
COPD = chronic obstructive pulmonary disease; CVD = cardiovascular disease; MI = myocardial infarction.
In a comparison of citywide COVID-19 hospitalization rates prior to and during the program, COVID-19 mortality decreased from 6.8% before the program with prophylactic use of ivermectin, to 1.8% after its beginning (RR, 0.27; 95% CI, 0.21-0.33; p < 0.0001), and in COVID-19 mortality rate, from 3.4% to 1.4% (RR, 0.41; 95% CI, 0.31-0.55; p < 0.0001) (Table 4).
| Overall | Until July 30th | After July 30th | Relative risk ratio (95% CI) | p-value | |
| Infected COVID-19 population (n) | 9,956 | 2,663 | 7,293 | - | - |
| Infected non-hospitalized COVID-19 population (n) | 9,641 | 2,481 | 7,160 | - | - |
| Hospitalized COVID-19 population (n) | 315 | 182 | 133 | - | - |
| COVID-19 hospitalization rate COVID-19 (%) | 3.2% | 6.8% | 1.8% | 0.27 (0.21-0.33) | <0.0001 |
| Overall number of COVID-19 deaths | 192 | 90 | 102 | - | - |
| Overall mortality rate (%) | 1.9% | 3.4% | 1.4% | 0.41 (0.31-0.55) | <0.0001 |
Table 4: Hospitalization and mortality rates registered in the city of Itajaí, Brazil, before versus after the beginning of the citywide program with ivermectin use as prophylaxis for COVID-19, independent of the ivermectin use status.
Discussion
This prospective, citywide COVID-19 ivermectin prophylaxis program resulted in significant reductions in COVID-19 infections, hospitalizations, and deaths. The ivermectin non-users were two times more likely to die of COVID-19 than ivermectin users in the overall population analysis. Since groups were compared for the exposure during the same period, in a parallel manner, changes in transmission rates would affect ivermectin users and non-users equally.
The city of Itajaí, in the state of Santa Catarina, Brazil, started a citywide program of prophylaxis with ivermectin in July 2020 as part of several initiatives to reduce the burden of COVID-19. The use of ivermectin was based on the existing literature at that time and on the virtual absence of risks. The National Health System (SUS) functions as full healthcare support to the entire population allowed the city to establish a non-restricted population program. This program included a support structure consisting of a large outpatient clinic located at the Convention Center of Itajaí. This outpatient clinic became the main locale of assistance for COVID-19 patients, supported by multiple public facilities where general practitioners regularly saw patients.
The use of ivermectin was optional unless contraindicated and given upon medical discretion. A structured medical-based program with a medical visit and evaluation of basic demographic characteristics and comorbidities offered ivermectin as optional prophylaxis to those who agreed to participate in this preventive treatment program. Health status was assessed and data were entered prospectively throughout the period of the program, in a fully digitized system provided by the National Health System (SUS). Since the system existed prior to the pandemic, a significant number of the population were already registered with their health information, including past and current diseases, use of medications, and other characteristics. The adaptations made to the SUS for the pandemic preparedness, prior to the initiation of this ivermectin outpatient program, allowed a structured, well-organized collection of the data that monitored any missing values, reinforcing the reliability of the results.
An important conservative bias was present. Major risk factors for severe COVID-19 and mortality due to COVID-19, including aging, diabetes, and hypertension, were more present among ivermectin users, which may have underestimated the benefits of ivermectin as it was demonstrated to be particularly effective in subjects above 49 years old in terms of reduction of absolute risk, which corresponds to the group at the highest risk for COVID-19. This allows the understanding that prophylactic use of ivermectin can be particularly impactful in older subjects. In addition, ivermectin seemed to reduce the exceeding risk of hypertension, T2D, and other diseases.
In accordance with the literature, subjects with higher age, diabetes, and males were less likely to survive (p < 0.05 for all), and only aging remained as an independent risk factor after PSM (p < 0.0001). However, prophylactic ivermectin use appears to mitigate the additional risk of COVID-19 death due to T2D, hypertension, and cardiovascular diseases.
The narrative that using preventive and early treatment therapies will have people relax their caution of remaining socially and physically distanced to allow more COVID-19-related infections is not supported here. These study data demonstrate that the use of preventive ivermectin significantly lowers the infection rate and that benefits outweigh the speculated increased risk of changes in social behaviors. Hence, we can speculate that the prophylactic use of ivermectin could play an important role in the reduction of the pandemic burden.
Even after adjustments to measure the most relevant variables that could influence COVID-19-related outcomes, including age, sex, comorbidities, and habits, aiming to avoid overestimation of the effects of ivermectin and to resemble a randomized clinical trial, prophylactic ivermectin proved to be protective for the overall population, with a reduction of 68% in mortality rate and p < 0.0001 after employment of PSM.
The protection provided by ivermectin when used prophylactically for COVID-19 may have reflected in the reduction in COVID-19 hospitalization and mortality rates observed at a population level. Compared to before the beginning of the program, COVID-19 hospitalization and mortality rates were reduced by 73% and 59%, respectively (p < 0.0001 for both). These reductions were obtained when the overall population and the number of COVID-19 cases, hospitalizations, and deaths in the city of Itajaí were considered, irrespective of the percentage of patients using ivermectin prophylactically. There were no changes in SARS-CoV-2 variants, infectivity, and pathogenicity before and during the program.
When compared to all other major cities in the state of Santa Catarina, differences in COVID-19 mortality rate before July 7, 2020, and between July 7, 2020, and December 21, 2020, Itajaí was ranked number one [35]. These results indicate that medical-based optional prescription and citywide covered ivermectin can have a positive impact on the healthcare system. However, the present results do not provide sufficient support for the hypothesis that ivermectin could be an alternative to COVID-19 vaccines.
Due to a large number of participants, this citywide program was unable to supervise whether ivermectin users were using ivermectin regularly, although the accumulated number of ivermectin tablets was strictly controlled. This occurred to be a potential conservative bias since the effects of ivermectin on prophylaxis could be underestimated due to adherence to the recommended frequency of ivermectin use.
While ivermectin is a multi-target drug [36], its maximum benefits occur when it is present at a minimum concentration in a wide range of sites to inhibit multiple metabolic and inflammatory pathways. However, although the dose of ivermectin employed in the program was smaller than the minimum to reach the concentration required to act in these multiple sites, the reduction in infection, mortality, and death rates in the infected group that used ivermectin prophylactically was surprisingly lower. Long-term or accumulated ivermectin could also play a critical role in its long-term protection against COVID-19.
Limitations
Being a prospective observational study that allowed subjects to self-select between treatment vs. non-treatment instead of relying on randomization, important confounders may have been differentially present, which could otherwise explain the differences observed. Given that the benefits measured occurred despite negative risk factors being more present in the treatment group, this suggests the benefits are likely accurate and unbiased. Further, studies relying on PSM techniques have been shown to consistently agree with those employing randomization [37,38], again supporting the likelihood that the benefits measured are accurate. The prevailing type of SARS-CoV-2 in the city was unknown due to the lack of genotyping surveillance during the period of the program. Whether the prophylaxis proposed in this program would be as effective in other SARS-CoV-2 variants is unclear. Also, there was no strict control on whether infected subjects used any specific drug in case of COVID-19 infection, and this allows the possibility that the differences may be explained by differences in the use of ivermectin or other medications as treatment.
Final discussion
In this citywide ivermectin prophylaxis program, a large, statistically significant decrease in mortality rate was observed after the program began among the entire population of city residents. When comparing subjects that used ivermectin regularly, non-users were two times more likely to die from COVID-19 while ivermectin users were 7% less likely to be infected with SARS-CoV-2 (p = 0.003).
Although this study is not a randomized, double-blind, placebo-controlled clinical trial, the data were prospectively collected and resulted in a massive study sample that allowed adjustment for numerous confounding factors, thus strengthening the findings of the present study.
Due to the well-established, long-term safety profile of ivermectin, with rare adverse effects, the absence of proven therapeutic options to prevent death caused by COVID-19, and lack of effectiveness of vaccines in real-life all-cause mortality analyses to date, we recommend that ivermectin be considered as a preventive strategy, in particular for those at a higher risk of complications from COVID-19 or at higher risk of contracting the illness, not as a substitute for COVID-19 vaccines, but as an additional tool, particularly during periods of high transmission rates.
Conclusions
In a citywide ivermectin program with prophylactic, optional ivermectin use for COVID-19, ivermectin was associated with significantly reduced COVID-19 infection, hospitalization, and death rates from COVID-19.
References
- Chen IS, Kubo Y: Ivermectin and its target molecules: shared and unique modulation mechanisms of ion channels and receptors by ivermectin. J Physiol. 2018, 596:1833-45. 10.1113/JP275236
- Kaur H, Shekhar N, Sharma S, Sarma P, Prakash A, Medhi B: Ivermectin as a potential drug for treatment of COVID-19: an in-sync review with clinical and computational attributes. Pharmacol Rep. 2021, 73:736-49. 10.1007/s43440-020-00195-y
- Martin RJ, Robertson AP, Choudhary S: Ivermectin: an anthelmintic, an insecticide, and much more. Trends Parasitol. 2021, 37:48-64. 10.1016/j.pt.2020.10.005
- Mastrangelo E, Pezzullo M, De Burghgraeve T, et al.: Ivermectin is a potent inhibitor of flavivirus replication specifically targeting NS3 helicase activity: new prospects for an old drug. J Antimicrob Chemother. 2012, 67:1884-94. 10.1093/jac/dks147
- Wagstaff KM, Sivakumaran H, Heaton SM, Harrich D, Jans DA: Ivermectin is a specific inhibitor of importin α/β-mediated nuclear import able to inhibit replication of HIV-1 and dengue virus. Biochem J. 2012, 443:851-6. 10.1042/BJ20120150
- Crump A: Ivermectin: enigmatic multifaceted 'wonder' drug continues to surprise and exceed expectations. J Antibiot (Tokyo). 2017, 70:495-505. 10.1038/ja.2017.11
- Heidary F, Gharebaghi R: Ivermectin: a systematic review from antiviral effects to COVID-19 complementary regimen. J Antibiot (Tokyo). 2020, 73:593-602. 10.1038/s41429-020-0336-z
- Li N, Zhao L, Zhan X: Quantitative proteomics reveals a broad-spectrum antiviral property of ivermectin, benefiting for COVID-19 treatment. J Cell Physiol. 2021, 236:2959-75. 10.1002/jcp.30055
- Jin L, Feng X, Rong H, et al.: The antiparasitic drug ivermectin is a novel FXR ligand that regulates metabolism. Nat Commun. 2013, 4:1937. 10.1038/ncomms2924
- Yang JS, Qi W, Farias-Pereira R, Choi S, Clark JM, Kim D, Park Y: Permethrin and ivermectin modulate lipid metabolism in steatosis-induced HepG2 hepatocyte. Food Chem Toxicol. 2019, 125:595-604. 10.1016/j.fct.2019.02.005
- Cairns DM, Giordano JE, Conte S, Levin M, Kaplan DL: Ivermectin promotes peripheral nerve regeneration during wound healing. ACS Omega. 2018, 3:12392-402. 10.1021/acsomega.8b01451
- Zheng YY, Ma YT, Zhang JY, Xie X: COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020, 17:259-60. 10.1038/s41569-020-0360-5
- Nagai H, Satomi T, Abiru A, et al.: Antihypertrophic effects of small molecules that maintain mitochondrial ATP levels under hypoxia. EBioMedicine. 2017, 24:147-58. 10.1016/j.ebiom.2017.09.022
- Park A, Iwasaki A: Type I and type III interferons - induction, signaling, evasion, and application to combat COVID-19. Cell Host Microbe. 2020, 27:870-8. 10.1016/j.chom.2020.05.008
- Zhang X, Song Y, Ci X, et al.: Ivermectin inhibits LPS-induced production of inflammatory cytokines and improves LPS-induced survival in mice. Inflamm Res. 2008, 57:524-9. 10.1007/s00011-008-8007-8
- Okeahialam BN: Serine protease inhibitors could be of benefit in the treatment of COVID-19 disease. Ther Adv Infect Dis. 2021, 8:10.1177/20499361211032048
- Matsuyama T, Kubli SP, Yoshinaga SK, Pfeffer K, Mak TW: An aberrant STAT pathway is central to COVID-19. Cell Death Differ. 2020, 27:3209-25. 10.1038/s41418-020-00633-7
- Wang K, Gao W, Dou Q, Chen H, Li Q, Nice EC, Huang C: Ivermectin induces PAK1-mediated cytostatic autophagy in breast cancer. Autophagy. 2016, 12:2498-9. 10.1080/15548627.2016.1231494
- Dou Q, Chen HN, Wang K, et al.: Ivermectin induces cytostatic autophagy by blocking the PAK1/Akt axis in breast cancer. Cancer Res. 2016, 76:4457-69. 10.1158/0008-5472.CAN-15-2887
- Layhadi JA, Turner J, Crossman D, Fountain SJ: ATP evokes Ca2+ responses and CXCL5 secretion via P2X4 receptor activation in human monocyte-derived macrophages. J Immunol. 2018, 200:1159-68. 10.4049/jimmunol.1700965
- Juarez M, Schcolnik-Cabrera A, Dueñas-Gonzalez A: The multitargeted drug ivermectin: from an antiparasitic agent to a repositioned cancer drug. Am J Cancer Res. 2018, 8:317-31.
- Andersson U, Ottestad W, Tracey KJ: Extracellular HMGB1: a therapeutic target in severe pulmonary inflammation including COVID-19?. Mol Med. 2020, 26:42. 10.1186/s10020-020-00172-4
- Yan S, Ci X, Chen N, et al.: Anti-inflammatory effects of ivermectin in mouse model of allergic asthma. Inflamm Res. 2011, 60:589-96. 10.1007/s00011-011-0307-8
- Reis TA, Oliveira-da-Silva JA, Tavares GS, et al.: Ivermectin presents effective and selective antileishmanial activity in vitro and in vivo against Leishmania infantum and is therapeutic against visceral leishmaniasis. Exp Parasitol. 2021, 221:108059. 10.1016/j.exppara.2020.108059
- Scheim D: Ivermectin for COVID-19 treatment: clinical response at quasi-threshold doses via hypothesized alleviation of CD147-mediated vascular occlusion. [PREPRINT]. SSRN J. 2020, 10.2139/ssrn.3636557
- Ci X, Li H, Yu Q, et al.: Avermectin exerts anti-inflammatory effect by downregulating the nuclear transcription factor kappa-B and mitogen-activated protein kinase activation pathway. Fundam Clin Pharmacol. 2009, 23:449-55. 10.1111/j.1472-8206.2009.00684.x
- Zaidi AK, Dehgani-Mobaraki P: The mechanisms of action of Ivermectin against SARS-CoV-2: an evidence-based clinical review article. [PREPRINT]. J Antibiot (Tokyo). 2021, 10.1038/s41429-021-00430-5
- Kalfas S, Visvanathan K, Chan K, Drago J: The therapeutic potential of ivermectin for COVID- 19: a systematic review of mechanisms and evidence. [PREPRINT]. medRxiv. 2020, 10.1101/2020.11.30.20236570
- Behera P, Patro BK, Singh AK, et al.: Role of ivermectin in the prevention of SARS-CoV-2 infection among healthcare workers in India: a matched case-control study. PLoS One. 2021, 16:e0247163. 10.1371/journal.pone.0247163
- Hellwig MD, Maia A: A COVID-19 prophylaxis? Lower incidence associated with prophylactic administration of ivermectin. Int J Antimicrob Agents. 2021, 57:106248. 10.1016/j.ijantimicag.2020.106248
- World Medical Association. Declaration of Helsinki. (2020). Accessed: December 24, 2021: https://www.wma.net/what-we-do/medical-ethics/declaration-of-helsinki/doh-oct2000/.
- Conselho Federal de Medicina (CFM). Código de Ética Médica. (2010). Accessed: December 24, 2021: https://portal.cfm.org.br/images/stories/biblioteca/codigo%20de%20etica%20medica.pdf.
- Nguyen TL, Collins GS, Spence J, Daurès JP, Devereaux PJ, Landais P, Le Manach Y: Double-adjustment in propensity score matching analysis: choosing a threshold for considering residual imbalance. BMC Med Res Methodol. 2017, 17:78. 10.1186/s12874-017-0338-0
- Zhang Z, Kim HJ, Lonjon G, Zhu Y: Balance diagnostics after propensity score matching. Ann Transl Med. 2019, 7:16. 10.21037/atm.2018.12.10
- Boletim epidemiológico do estado de Santa Catarina, Brasil. (2020). Accessed: December 24, 2021: http://www.dive.sc.gov.br.
- Choudhury A, Das NC, Patra R, Bhattacharya M, Ghosh P, Patra BC, Mukherjee S: Exploring the binding efficacy of ivermectin against the key proteins of SARS-CoV-2 pathogenesis: an in silico approach. Future Virol. 2021, 16:277-91. 10.2217/fvl-2020-0342
- Austin PC: An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011, 46:399-424. 10.1080/00273171.2011.568786
- Propensity score matching in the absence of randomized controlled trials: a case study on the effects of breastfeeding on childhood obesity. (2020). Accessed: December 24, 2021: https://methods.sagepub.com/case/propensity-score-matching-trials-effects-breastfeeding-childhood-obesity.
https://www.canadiancovidcarealliance.org/
https://www.skirsch.io/how-to-treat-covid/
This article primarily covers treating COVID, long-haul COVID, and side-effects from COVID vaccines. We also talk about the Together trial results, why clinical trials fail, etc. We include COVID prophylaxis and early treatments that do not currently require a prescription because in many countries the prescription drugs may not be available.
Disclaimer: This info is for educational purposes only. Please consult with your doctor before taking any drugs.
If you have to get a vaccine, which one is the safest?
Pfizer, then Moderna, then J&J. See Vaccine risk benefit by age.
How to avoid vaccine side effects
- Many people will try to get Sinovac-CoronaVac or Sinopharm. The vaccine doesn't work, but there are no side effects and you get your vaccine card which is the important thing. But it may not be "usable" in other countries.
- If you are forced to get one of the US vaccines, using .2mg/kg of ivermectin the day before, the day of, and the day after will reduce your chance of side effects by 95% according to a prominent researcher in Brazil we know. Of course, the FDA and AMA are trying their best to block your access to ivermectin, a new low for medicine. The mainstream medical community are cheering them on.
Treating COVID
Got COVID? Treating it ASAP is key for best outcomes. Even if it seems mild at first, treat COVID like you'd treat a fire in your house: the sooner you put it out, the less the long term damage.
Remember: The only thing all the COVID patients in hospitals today have in common today is that they didn't treat their infection using a proven early treatment protocol (or they waited too long).
Step 1: Find a doc, get a prescription, and get the medications filled now so that they can be on hand for your immediate use. This is critical for new variants because every hour counts. In some cases, you may need to have another condition in order to get a prescription, e.g., if you have OCD, you can get fluvoxamine for that condition and the use for COVID is a nice fringe benefit. There are also some treatments that don't require a prescription.
Step 2: As soon as you think you might have COVID, start treatment. Don't wait for a positive test. If your test result ends up being negative, stop the treatment. Because the treatments are so safe, everyone, even kids, can and should be treated immediately upon suspected COVID. Early treatment reduces risk of hospitalization, death, and reduces the chance of getting long-haul COVID which can be very hard to treat. If you started treatment early, your symptoms should start reversing about 24 hours after you start treatment.
List of doctors
Your doctor is unlikely to know how to treat you correctly. Here is a list of telemedicine providers who know their stuff and will give you a prescription for you to fill now so that you will have ALL the drugs on hand if/when you get sick. This is important because you want to have all the drugs immediately available. Time is critical.
List of doctors who will write early treatment COVID prescriptions
They generally will prescribe to you one of the following early treatment protocols or some modification that they personally like. Each physician ends up using his own judgement based on what they've personally seen work the best.
- Modified Patterson protocol (shown below)
- I-MASK+ protocol from flccc.net. See this Chris Martenson video.
- Tyson-Fareed protocol: Has 99.76% risk reduction and no safety downsides.
- Zelenko early treatment protocol: Another highly effective treatment.
- Chetty protocol: Described in this paper, it has over 99% risk reduction.
- Italy protocol: This is extremely effective. Reportedly, only 4 out of 66,000 people died in Italy. This is an HCQ-based protocol because ivermectin is prohibited in Italy.
- Egyptian protocol: Very successful in Egypt
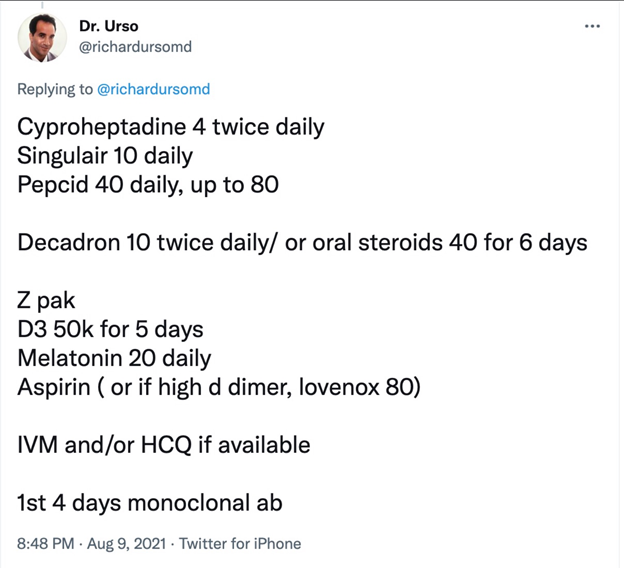
- Dr. Urso protocol (the lack of units is a bit troubling):
Modified Patterson early treatment protocol for COVID
Based on recommendation of Dr. Bruce Patterson with a few minor improvements. Patterson who treats thousands of long-haul COVID and vaccine cases so he knowns more than anyone else the drugs that in combination are the most effective in countering the inflammation caused by COVID. Take all drugs (that you can access) IMMEDIATELY after you suspect a COVID infection (except as indicated). The following are all safe and do not interact with each other.
- Fluvoxamine (luvox) 50mg twice a day for 14day. If not available, use fluoxetine (prozac) 30mg once a day x 14 days. If already on an antidepressant, consider talking to your doctor about switching. Avoid caffeine, alcohol, tylenol, and benadryl while on fluvoxamine. Fluvoxamine prevents brain fog because it passes through the blood brain barrier. In rare cases, can cause hair loss. If you can't tolerate fluvoxamine, try Prozac instead. It works just as well (proven in multiple observational studies). If you are jittery, have dilated pupils, or other side effects, you may need to reduce the dosage. For details on fluvoxamine, see My substack article on fluvoxamine.
- Ivermectin .4 mg/kg every day for a minimum of 10 days and continue until symptoms resolved. Take with a meal or right after a meal for best absorption. Ivermectin is one of the safest drugs ever invented. See the FLCCC website for more info. Some people are super sensitive and can't take that dose every day. In that case, taking it every 3 days should be fine since it is slowly eliminated from your body.
- Inhaled budesonide: 400 µg per actuation (two puffs to be taken twice per day; total dose per day 1600 µg) x 14 days (or until resolution of respiratory symptoms). You really want to throw the kitchen sink at this virus and the number one reason people got to the hospital is respiratory distress. The latest Together trial will be testing fluvoxamine and budesonide in combination. We recommend this even if you don't appear to have any respiratory symptoms because you want to play it safe and keep it that way.
- NAC: 600mg/day for 14 days. This mitigates the damage caused by the spike protein. This is a super safe drug that was available over the counter for 60 years. After 60 years of safety, and incorporation in 1,500 products, it was made prescription only so people would not have access to it and would be forced to get vaccinated.
- Vitamin D3: 15,000 IU/day for 14 days to lower inflammation.
- Pravastatin: 20mg x 14 days. Other statins can be used but this is the best.
Early-treatment "options"
Here are a few optional "add-ons" that you can safely add to any of the protocols that can make a difference (if not already in your protocol). You can even do quite well using these as your only defense. Although all are available without a prescription, always discuss with your doctor before taking these. They can be considered if you cannot adopt a proven combo protocol or you simply want an extra margin of protection.
It is not always the case that more is better. You can run into weird interactions when taking lots of drugs at the same time.
- Benadryl + lactoferrin: Take as soon as you have symptoms. Both are very safe and available without a prescription. Together they are 99% effective according to this article. Here is the paper. CAUTION: Do not combine benadryl and fluvoxamine; they interact. Benadryl can cause your eyes to dilate.
- Aspirin: Reduces chance of death by around 50%. Either size works. Take once a day for 10 days after first symptoms.
- Nigella sativa (no prescription needed)
Black seeds 40mg/kg orally once per day for 14 days. $9 gets you a 70 day supply. Reduces hospitalization risk by 75%. Death by 95% . - Vitamin D3: 15,000 IU/day for 14 days to lower inflammation. Up to 80% reduced risk. Ideally, you'll want to take with magnesium for complete absorption. Also, if you try to load up AFTER you get COVID, it will take too long unless you pre-order this and have it on hand: d.velop Vitamin D.
- Povidone-iodine (Betadine): .5% to 1% solution (no prescription needed; widely available at drug stores at low cost). Do it 3 times a day for the first 3 days. The 1% will be somewhat uncomfortable. The .5% will hurt less. So if you can't tolerate the 1%, dilute it down 1:1 with purified water.
The pro tip is to buy the 10% solution and then dilute it down to 1% or even .5%. Otherwise you'll be sorry. So a bottle of the 10% solution (which will cost you around $15 or less for an 8oz container) is going to last you a LONG LONG time.
Mouthwash/gargle and nasal drops (or rinse) 3 times a day starting on first symptoms. After 7 days you'll see a 99% drop in viral load and you'll lower your risk of death by nearly 90%. See Effect of 1% Povidone Iodine Mouthwash/Gargle, Nasal and Eye Drop in COVID-19 patients and Rapid initiation of nasal saline irrigation: hospitalizations in COVID-19 patients randomized to alkalinization or povidone-iodine compared to a national dataset which shows that early treatment can reduce your risk by 95% if you start early for just this one simple, easy, very safe intervention. You can get both solutions on Amazon or at www.immunemist.com. DO NOT USE THIS EVERYDAY as a prophylaxis. Instead, use within 12 hours of higher risk contact, or twice a day for 14 days if you get infected with COVID. It's basically a stronger solution than the hypertonic saline solution. - Colgate Total (no prescription needed)
Total contains cetyl pyridinium chloride (CPC). Within 12 hours after possible contact, swish and gargle for 30 seconds and put a saturated Qtip up your nose (watch this instructional video). You can use other mouthwashes with CPC. This is a very simple and inexpensive solution to the problem ($5 per month) that protects you against other viruses as well. - Hypertonic saline solution nasal rinse (no prescription needed)
Create a hypertonic solution by adding 1 tsp of salt (5g) to 8oz water. This will create a 2% solution. Do a nasal rinse with a squeeze bottle (I use the 8 oz NeilMed squeeze bottle) or a neti pot. If you do the rinses occasionally (because you are rarely exposed), the NeilMed bottle is fine. If you do more often, the neti pot is better since there is no pressure so less potential damage to sensitive nasal structures. Do this within 12 hours after a risky incident (e.g., before bed). For extra credit, with remaining hypertonic solution, gargle, swish and then spit after 20-30 seconds. However, most COVID infections are through the nose. A lot of doctors say you should use purified or distilled water. Others I highly respect say that's overkill and say tap water is fine. I've always used warm tap water (at same temperature as your body temperature) and never had a problem. Compliance is the most important factor. - NAC: 600mg/day for 14 days. This mitigates the damage caused by the spike protein. This is a super safe drug that was available over the counter for 60 years. After 60 years of safety, and incorporation in 1,500 products, it was made prescription only so people would not have access to it and would be forced to get vaccinated. I bought mine at Thorne. No prescription needed.
- Glutamine: 10 g l-Glutamine available in powder forms were given 3 times a day with meals. In the control group, 38 out of 230 covid patients died. In the glutamine group, 0 out of 222 patients died:The effect of glutamine supplementation on serum levels of some inflammatory factors, oxidative stress, and appetite in COVID-19 patients: a case-control study - PubMed (nih.gov) Again, no mortality and no ICU admission in the glutamine group… Effect of oral l-Glutamine supplementation on Covid-19 treatment - PubMed (nih.gov)
Prophylaxis protocols (recommended)
Lactoferrin (no prescription needed)
"“We found lactoferrin had remarkable efficacy for preventing infection, working better than anything else we observed," Sexton said. He adds that early data suggest this efficacy extends even to newer variants of SARS-CoV2, including the highly transmissible Delta variant.” This is safe.
However, it may be more convenient just to skip the prophylaxis, get COVID, and treat it early.
Prophylaxis protocols (not recommended)
FLCCC prophylaxis protocol
This is an ivermectin-based protocol. However, in consultation with other docs (gut specialists), I do not recommend it because it will destroy the good bacteria in your gut. In general, do not take prescription drugs for prophylaxis.
Nasal irrigation (no prescription needed)
Done twice a day has been remarkably effective in preventing COVID infections. See hypertonic above for details. Again, this is NOT recommended because you will upset the bacteria balance in your nose. If you do it, you only want to treat on an acute basis (i.e., when you are sick).
Other drugs that work against COVID-19
See C19 Early for a list of drugs and effect sizes.
Treating long haul COVID
Bruce Patterson’s long haul COVID treatment relies on four drugs. The dosing depends on what your bloodwork shows (based on the Cytokine 14 panel available at covidlonghaulers.com), so the dosages are averages.
- Fluvoxamine: 50mg BID
- Ivermectin: .2mg/kg every 3 days
- Pravastatin: 20mg (substitute for fractal kinase inhibitor)
- Maraviroc 300mg PO BID. This reduces CCR5 and takes about 5 days to work.
The other option is going to covidlonghaulers.com and getting tested. Then they'll prescribe drugs based on your test results.
Treating pre- and Post-Vaccine Inflammatory Syndrome (PVIS)
Ideally start this 3 days before you vaccinate. Less ideally, start this immediately after vaccination.
Continue for 14 days if using to minimize vaccine side effects.
The longer you wait, the more likelihood of permanent damage to heart, lungs, and brain. Once those tissues are scarred from inflammation, they will never heal. This is why many long-haulers never regain full function. It's exactly the same story with vaccine victims. Watch this 8 minute video featuring Dr. Charles Hoffe.
- Fluvoxamine: 50mg BID (can substitute 30mg Prozac QD)
- Ivermectin: .2mg/kg daily. You may see results in less than 24 hours. Note this is a lower dose than an active COVID infection.
- Prednisone: 5mg/day for inflammation. Note: this is a low amount because if you give more you start to affect the immune system which is problematic because you want the macrophages to clear out the spike protein
- Pravastatin: 20mg (substitute for fractal kinase inhibitor)
- Maraviroc 300mg PO BID. This reduces CCR5 and takes about 5 days to work.
For best results, go to covidlonghaulers.com and getting tested with the 14 cytokine panel and they'll prescribe the appropriate drugs based on your test results (since the Maraviroc is pretty pricey). You also will want to get the Spike Protein test at incelldx.com (but it seems it isn't available as of Sept 7, 2021).
Or check out the FLCCC I-Recover protocol; it can be used for PVIS as well (as they note in the text).
Drugs that may be available in the future
These drugs will be difficult to impossible to obtain currently in the US but may be available in other countries:
- enovid. This drug is made by SaNOtize . It probably won't be available in your area, but it appears to be effective.
- Interferon Lambda: If you can get a single injection of Interferon Lambda (made by Eiger), that is the drug with the largest effect size and best safety profile. It is currently only available in clinical trials. It should be taken ASAP after infection for best results. It drastically reduces d-dimer which is an excellent indication that has a dramatic effect in lowering blood clotting (and likely inflammation). You basically will not get hospitalized if you get this drug. If you only can take one drug, this is the drug to take. If you can get access to this drug early, everything else is optional.
- Camostat: 200mg taken orally, 4 times daily, for 7 days will absolutely reduce your chance of long haul COVID symptoms and reduce your risk of hospitalization. It isn't approved in the US, but is approved in other countries. It will not change your time to recover. It's about preventing you from developing long-haul COVID symptoms and severe disease. It's an antiviral so take ASAP.
- Proxalutamide: Appears extremely impressive, near 100% efficacy. Now in Phase 3 trials in USA.
Currently, the five most effective drugs for COVID are:
- Interferon lambda
- Fluvoxamine or Fluoxetine (Prozac)
- Ivermectin
- Inhaled budesonide (see this tweet)
- Camostat
That list was made on July 26, 2021. It will be 4 months before the rest of the world figures it out.
Note about Together trial results for fluvoxamine and ivermectin
Why did Ivermectin seem to fail and Fluvoxamine not do so well? Ivermectin was dosed for 3 days; fluvoxamine for 10 days.
We don't think the trial was gamed at all. I think this was a legit result.
We know the PI Edward Mills and believe he is totally honest and we have no reason not to believe the results he obtained. But we also believe other researchers as well.
So the question everyone has is how could these drugs do so well in other studies?
The answer: the variant was different. P1 is the variant in Brazil and makes Delta look like a walk in the park. If you do not treat P1, instantly upon symptoms, you will see big failures.
Had fluvoxamine been given on Day 0 instead of Day 4, there would have been a dramatically different result.
Had ivermectin been dosed at .6mg/day for 14 days starting on Day 0 (the first day of symptoms), there would have been a dramatically different result.
The more aggressive the variant, the earlier and harder you have to treat it.
Ivermectin likely failed for these five reasons:
- Too little a dose
- Started too late
- Not taken with meal or shortly after
- Not continued for long enough
- Many patients may have already been taking ivermectin
The healthcare systems need to encourage people to have the meds in the cabinet for immediate use. Nobody does that. That's why we have a problem.
Also, you can't treat Delta and P1 in the hospital... it is much much tougher there. It's like a fire department arriving when the entire building is in flames.
Early aggressive treatment is key. There are near ZERO hospitalizations and DEATHs for anyone treated early. But the press never talks about that. The NIH or CDC never says that either. Why not?
You can't say vaccination works: at Mt Sinai in NY, 27% of the hospitalized cases are vaccinated, and 17% of ICU patients are vaccinated.
The sooner we stop following the NIH advice that early treatments don't work, the sooner we will start saving lives.
Ways a clinical trial can fail
Clinical trials on repurposed drugs should always be tested first on outpatients by physicians who prescribe on a shared decision making basis. Once a protocol is found to be reliable, then it can be "locked" into a clinical trial for "proof" of efficacy. Sadly, we do the opposite which wastes a lot of time and money. We form a hypothesis and then invest millions to test it out in a large scale trial rather than on an outpatient basis.
Here are some ways a clinical trial can fail.
- Dose: standard dosing may need to be increased for new variants. The FLV dosing of 50mg BID was tested for alpha variant. In general, increase dose for aggressive variants or treatment that is started later after infection. In this trial they used 100mg BID. The downside is that this dose can lead to compliance problems where people have to discontinue the use of the drug.
- Timing: Ivermectin is best taken with a fatty meal or right after, not on an empty stomach. The FDA however requires the drug to be taken on an empty stomach in trials due to worries about liver toxicity, even though this hasn't been a problem in any other trial. This seems very silly.
- Treatment delay: Treatment in Together started on average 4 days after symptoms. Too long of a wait especially for fast replicating variants like Delta. The lesson is start treatment IMMEDIATELY after symptoms recognized or before, especially with aggressively replicating variants. This is the most important determinants of success; once the damage is done, it is hard to reverse. This is the most important thing to get right.
- Compliance: Patient compliance in the Together trial was estimated to be somewhere around 80%. If compliance is low, it is going to limit your effect size. How can the study prove that everyone took all their meds as directed? We can only see this by looking at the source data of the study for clues. As the pandemic continues, we've found patient compliance to drop dramatically. Early in the pandemic, you could call participants and talk to you. Today, you call and they hang up on you.
- Duration: Delta can hang around for 33 days. Treatment should be continued until 5 days after symptoms resolve. So shouldn't be a fixed duration (like it was in the trial). In the trial, the duration for ivermectin was only 3 days; was 10 days for fluvoxamine.
- Deception: Participants were supposed to be early in COVID, but many could have given inaccurate information either willfully or mistakenly. There was no way to tell because this wasn't measured. This explains how so many ended up in the hospital so fast (e.g., within 1 day after treatment started). There wasn't baseline bloodwork taken to assess disease state of the participants. They could have determined disease stage from this and better assessed outcomes.
- Lack of adaptability: Some doctors find that using D-dimer and CRP to guide the dose and duration can be very helpful. That is rarely done in a clinical trial.
- Single drug: Using a multi-drug protocol will work better especially if the drugs are synergistic. For example, many people claim HCQ without zinc is a non-starter.
- Tampering: Phase 3 trials don't have levels of controls to detect manipulation. It relies on everyone being trustable in doing their jobs. If the drugs are switched accidentally (placebo vs. real drug), no one will know. This is why it is important to look at the source data and the side effect reports. Even the best designed studies are susceptible to tampering. That tampering could be deliberate or accidental and it can be hard to detect.
- Data manipulation: One ivermectin study showing a positive result was clearly manipulated. Data manipulation does happen. It can sometimes take months before this is exposed.
- Controls may already be taking one of the study drugs: A major reason why ivermectin trials don't fare too well in S. America is that lots of controls may have taken ivermectin. For example, in the TOGETHER trial, it was NOT an exclusion criteria (and so the data should be segmented by that before coming to conclusions).
- Dropouts. People can drop out of the trial causing you to lose statistical power.
- Missing data. People can not report back what happened.
- Low event rate. You may underpower the trial because people are healthier than you presumed or the virus mutates to a less dangerous strain.
- Competitive sabotage. A competitor can pay enrollees to enroll in the trial and not take the drug.
These are issues that can come up with any trials, even well done trials. It's a shame these trials in general do not have more controls to detect these mistakes. They happen. This is a known limitation of every clinical trial; few if any have any robustness to errors.
One other very important point is that researchers are PROHIBITED by their IRB and other entities from testing ivermectin doses and durations that would be effective! One doctor in the US just told me that they wouldn't let him go higher than 200mg/kg for 3 days. That's crazy. Ivermectin is one of the safest drugs on the planet.
An idea for rapidly screening drugs against COVID
The biggest problem with COVID is the inflammation and clotting. The vaccines create the same rise in CRP and D-dimer as COVID and it's very reliable (happens post-vax in over 60% of cases).
Therefore, if we want to test a single drug against COVID, all we need is 5 volunteers who have been recently vaccinated. Treat immediately after vaccination with the drug. Measure CRP and D-dimer at 5 days. If both are normal in all 5 patients in 5 days, you have a candidate drug.
Once you have 3 candidate drugs and test the combo in a clinical trial.
For more information
- Early treatment is key to better outcomes
- Detailed advice on treatment
- Ten things to know about treating COVID infections
- Drugs and dosages
- Summary of what we know about treating early (just read the introduction)
- Short summary of the case for using fluvoxamine for COVID (slides only)
- Video presentation of the slides: 15 minutes at start of Semmelweis effect seminar
- Detailed summary of the evidence supporting the use of fluvoxamine for COVID
The tl;dr is that every piece of evidence we have ever seen (observational studies, randomized trials, doctor experiences) is positive. There are no cases where fluvoxamine made things worse. If treated early enough with fluvoxamine, patients can recover and completely avoid long-haul COVID issues. - COVID-19 Early Treatment Fund (CETF) Introduction - YouTube
- Fluvoxamine: Finding a possible early treatment for COVID-19 in a 40-year-old antidepressant - 60 Minutes - CBS News
https://americanbuddhist.net/2021/12/13/france-covid-mortality-with-vs-without-hcq/
In a recent presentation, Pr. Million from IHU Marseille has presented their first numbers of Covid mortality by age group in 2021.
He has highlighted the improved 2021 mortality where patients did not get HCQ+AZ, which he attributed to the discreet introduction of Ivermectin.

IHU has adopted Ivermectin in 2021 but has stayed silent about it.
Possibly to avoid controversy and maintain access to the drug, and more likely because French regulators insisted that off-label use was a right but any publicity would be sanctioned.
- No labels
